Overview
Overview
A COMPARATIVE-EFFECTIVENESS STUDY ON EXPANSION CRANIOTOMY VERSUS DECOMPRESSIVE CRANIECTOMY FOR SURGICAL MANAGEMENT OF TRAUMATIC BRAIN INJURY IN PATIENTS WITH INTRACRANIAL COMPARTMENT SYNDROME.
Traumatic brain-injured (TBI) patients require often surgical management to reduce intracranial pressure (ICP). The most common procedures include external ventricular drain (ventriculostomy), basal cisterns drain (cisternostomy), expansion craniotomy (hinge craniotomy, floating craniotomy, etc.) or decompressive craniectomy (unilateral, bilateral, primary, secondary, bifrontal or unilateral) (1-4).
The common aspect of all these procedures (that can be used as a unique procedure or combined with the others), is to prepare the cranial vault for increasing compliance in cases where the physiological mechanisms for compensation are exhausted due to a mass effect caused by intracranial blood collections or brain tissue edema (5).
In general, from all the above-mentioned surgical procedures, cranial decompression has been proposed in most of the protocols of care as a third-line therapy for reducing the impact of an intracranial compartment syndrome. The intracranial compartment syndrome (ICCS) has been described as the compromise of neural and vascular tissue due to an increased pressure in one, two or all the three intracranial compartments (left and right supratentorial and infratentorial) (6-8).
Clinical studies focused on the analysis of decompressive craniectomy, have shown that cranial decompression (leaving the bone out of the skull, either in a bone bank or in a subcutaneous pocket at the abdominal area) can cause more complications at the operative site, including CSF leak, skin local infection, incision dehiscence, etc.) (9-12).
Due to these situations, expansion craniotomy techniques have been proposed also as a safer surgical alternative for restoring compliance of the cranial vault in TBI patients, reducing complications associated to the regular decompressive craniectomy procedure. The aim of this study is to determine the outcomes of decompressive craniectomy versus expansion craniotomy in the surgical management of patients with TBI and ICCS.
- Chau CYC, Craven CL, Rubiano AM, Adams H, Tülü S, Czosnyka M, Servadei F, Ercole A, Hutchinson PJ, Kolias AG. The Evolution of the Role of External Ventricular Drainage in Traumatic Brain Injury. J. Clin. Med. 2019, 8, 1422. https://doi.org/10.3390/jcm8091422.
- Cherian I, Bernardo A, Grasso G. Cisternostomy for Traumatic Brain Injury: Pathophysiologic Mechanisms and Surgical Technical Notes. World Neurosurg. 2016 May; 89:51-7. doi: 10.1016/j.wneu.2016.01.072.
- Layard Horsfall H, Mohan M, Devi BI, Adeleye AO, Shukla DP, Bhat D, Khan M, Clark DJ, Chari A, Servadei F, Khan T, Rubiano AM, Hutchinson PJ, Kolias AG. Hinge/floating craniotomy as an alternative technique for cerebral decompression: a scoping review. Neurosurg Rev. 2020 Dec;43(6):1493-1507. doi: 10.1007/s10143-019-01180-7.
- Rubiano AM, Carney N, Khan AA, Ammirati M. The Role of Decompressive Craniectomy in the Context of Severe Traumatic Brain Injury: Summary of Results and Analysis of the Confidence Level of Conclusions from Systematic Reviews and Meta-Analyses. Front Neurol. 2019 Oct 10; 10:1063. doi: 10.3389/fneur.2019.01063.
- Ocamoto GN, Russo TL, Mendes Zambetta R, Frigieri G, Hayashi CY, Brasil S, Rabelo NN, Spavieri Júnior DL. Intracranial Compliance Concepts and Assessment: A Scoping Review. Front Neurol. 2021 Oct 25; 12:756112. doi: 10.3389/fneur.2021.756112.
- Tonetti, T., Biondini, S., Minardi, F., Rossi, S., Picetti, E. (2021). Definition and Pathomechanism of the Intracranial Compartment Syndrome. In: Coccolini, F., Malbrain, M.L., Kirkpatrick, A.W., Gamberini, E. (eds) Compartment Syndrome. Hot Topics in Acute Care Surgery and Trauma. Springer, Cham. https://doi.org/10.1007/978-3-030-55378-4_2.
- Brogi, E., Coccolini, F., Russo, E., Forfori, F. (2021). Diagnosis and Treatment of the Intracranial Compartment Syndrome. In: Coccolini, F., Malbrain, M.L., Kirkpatrick, A.W., Gamberini, E. (eds) Compartment Syndrome. Hot Topics in Acute Care Surgery and Trauma. Springer, Cham. https://doi.org/10.1007/978-3-030-55378-4_3.
- Godoy DA, Brasil S, Iaccarino C, Paiva W, Rubiano AM. The intracranial compartmental syndrome: a proposed model for acute brain injury monitoring and management. Crit Care. 2023 Apr 10;27(1):137. doi: 10.1186/s13054-023-04427-4.
- Hutchinson PJ, Kolias AG, Timofeev IS, Corteen EA, Czosnyka M, Timothy J, Anderson I, Bulters DO, Belli A, Eynon CA, Wadley J, Mendelow AD, Mitchell PM, Wilson MH, Critchley G, Sahuquillo J, Unterberg A, Servadei F, Teasdale GM, Pickard JD, Menon DK, Murray GD, Kirkpatrick PJ; RESCUEicp Trial Collaborators. Trial of Decompressive Craniectomy for Traumatic Intracranial Hypertension. N Engl J Med. 2016 Sep 22;375(12):1119-30. doi: 10.1056/NEJMoa1605215.
- Hutchinson PJ, Adams H, Mohan M, Devi BI, Uff C, Hasan S, Mee H, Wilson MH, Gupta DK, Bulters D, Zolnourian A, McMahon CJ, Stovell MG, Al-Tamimi YZ, Tewari MK, Tripathi M, Thomson S, Viaroli E, Belli A, King AT, Helmy AE, Timofeev IS, Pyne S, Shukla DP, Bhat DI, Maas AR, Servadei F, Manley GT, Barton G, Turner C, Menon DK, Gregson B, Kolias AG; British Neurosurgical Trainee Research Collaborative, NIHR Global Health Research Group on Acquired
Brain and Spine Injury, and RESCUE-ASDH Trial Collaborators; RESCUE-ASDH Trial Collaborators. Decompressive Craniectomy versus Craniotomy for Acute Subdural Hematoma. N Engl J Med. 2023 Jun 15;388(24):2219-2229. doi: 10.1056/NEJMoa2214172. - van Essen TA, van Erp IAM, Lingsma HF, Pisică D, Yue JK, Singh RD, van Dijck JTJM, Volovici V, Younsi A, Kolias A, Peppel LD, Heijenbrok-Kal M, Ribbers GM, Menon DK, Hutchinson PJA, Manley GT, Depreitere B, Steyerberg EW, Maas AIR, de Ruiter GCW, Peul WC; CENTER-TBI Investigators and Participants. Comparative effectiveness of decompressive craniectomy versus craniotomy for traumatic acute subdural hematoma (CENTER-TBI): an observational cohort study. E-Clinical Medicine. 2023 Aug 9; 63:102161. doi: 10.1016/j.eclinm.2023.102161.
- Hawryluk GWJ, Rubiano AM, Totten AM, O'Reilly C, Ullman JS, Bratton SL, Chesnut R, Harris OA, Kissoon N, Shutter L, Tasker RC, Vavilala MS, Wilberger J, Wright DW, Lumba-Brown A, Ghajar J. Guidelines for the Management of Severe Traumatic Brain Injury: 2020 Update of the Decompressive Craniectomy Recommendations. Neurosurgery. 2020 Sep 1;87(3):427-434. doi: 10.1093/neuros/nyaa278.
Intracranial Compartment Syndrome
Intracranial Compartment Syndrome
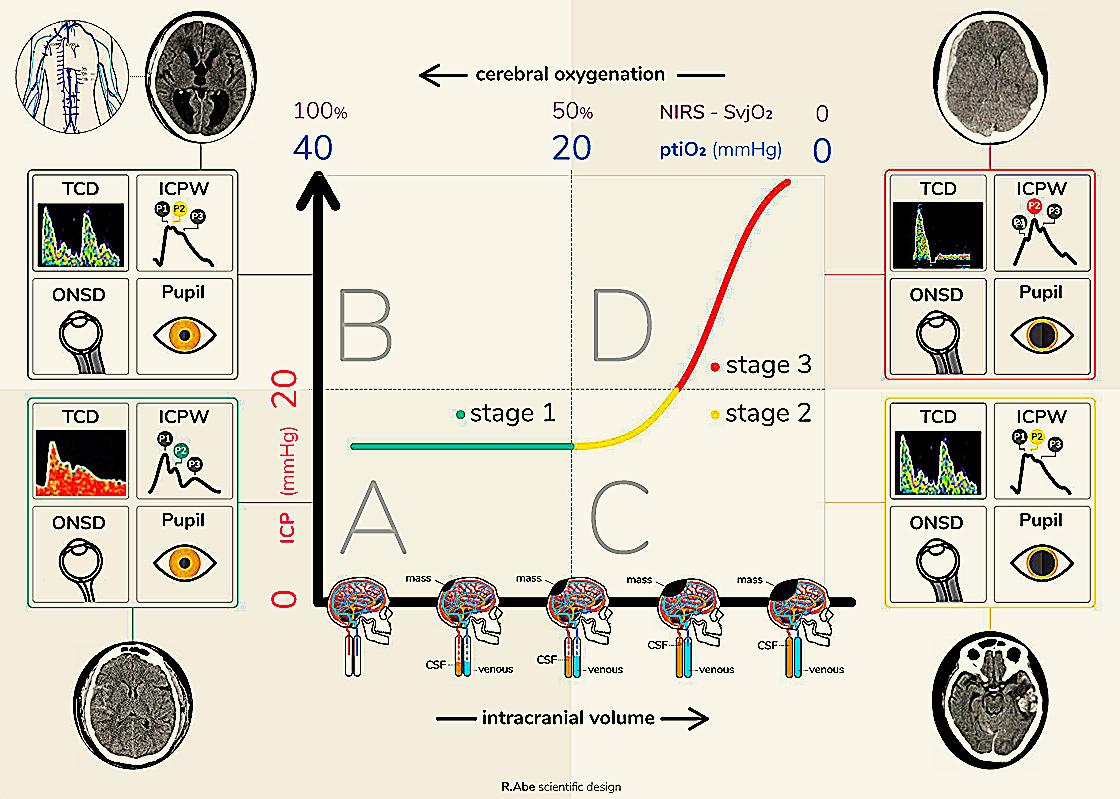
Intracranial compartment syndrome (ICCS) is a diagnostic model that identifies the loss of compliance in one or various cranial compartments. This corresponds to the point at which the compensatory mechanisms of intracranial pressure have been exhausted, leading to a compromised blood supply to the brain with subsequent ischemic cerebral injury.
The implementation of this model optimizes decision making for the treatment of patients with acute brain injuries since it allows the state of the intracranial compensatory reserve to be identified in a more integrated manner and to take into account individual variations that each patient may present that could modify the intracranial pressure threshold that is tolerated without injury to the brain tissue.
Analogous to how the management of intracranial hypertension is proposed, the treatment of ICCS has a tiered character, with cranial decompression surgical procedures considered as third-line measures to deal with the loss of cerebral compliance and prevent further brain ischemia.
Suggested readings:
- Rubiano, A. M., Figaji, A., & Hawryluk, G. W. (2022). Intracranial pressure management: moving beyond guidelines. Current opinion in critical care, 28(2), 101–110. https://doi.org/10.1097/MCC.0000000000000920
- Godoy, D. A., Brasil, S., Iaccarino, C., Paiva, W., & Rubiano, A. M. (2023). The intracranial compartmental syndrome: a proposed model for acute brain injury monitoring and management. Critical care (London, England), 27(1), 137. https://doi.org/10.1186/s13054-023-04427-4
- Godoy, D. A., Brasil, S., & Rubiano, A. M. (2024). Further support for the intracranial compartmental syndrome concept. Critical care (London, England), 28(1), 311. https://doi.org/10.1186/s13054-024-04974-4

Characteristics of the Study
Characteristics of the Study
This study will be a prospective, multicentric, observational, comparative-effectiveness enrolling patients from high developing index (HDI) regions and collecting also data in a group of countries from low and middle developing index (LMDI) regions. The data collection in these two different contexts, will allow understanding of the procedure´s impact in the outcome of patients from less resourced areas. This second group of countries will be identified as areas of “humanitarian research”.
The study will include patients with TBI and ICCS managed either by hemispheric expansion craniotomy or hemispheric decompressive craniectomy. Patients with pre-existing neurological disorders will be excluded. In an instrumental analysis, outcomes between centres according to treatment preference will be compared, measuring by the case-mix adjusted proportion per center. The primary outcome will be functional outcome rated by the Glasgow Outcome Scale Extended at discharge, 3 months, 6 months, and 12 months after surgery, estimated with ordinal regression as a common odds ratio (OR), adjusted for prespecified confounders. Variations between center preferences will be quantified with the median OR.
Demographic characteristics including vital signs, biochemical data, preoperative parameters at presentation, and intraoperative and postoperative variables will be collected from the study registry, including prehospital care, emergency care, surgical care, and intensive care data sections. The interviews for outcome evaluation will be performed on-site or by phone. Secondary outcomes will include aspects like control of the ICCS, frequency and type of neurosurgical interventions, medical and surgical treatment intensity, surgical site complications, ICU and in-hospital length of stay, including dichotomized GOSE score across multiple thresholds.





Expansion Craniotomy
Expansion Craniotomy
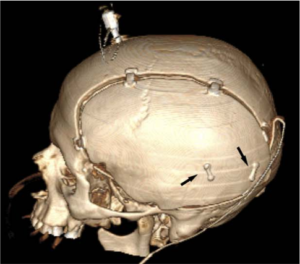
Expansion craniotomy is a specific surgical technique that allows certain degree of decompression whilst retaining the bone flap in situ, in a expanded fashion. This provides expansion potential for decreasing the impact of cerebral oedema whilst decreasing the complications of leaving the bone out of the skull. The exact indications, technique and outcomes of this procedure require more evidence, but it is likely that will provide a safety alternative technique to decompressive craniectomy (DC) in certain cases.

Registry
- ClinicalTrials.gov ID: NCT06776614
- ISRCTN ID: ISRCTN11229009

